Abstract
Background: Heparin-induced thrombocytopenia (HIT) is a rare disorder with potential to cause significant morbidity and mortality. Early identification and initiation of non-heparin anticoagulation can prevent devastating thrombotic events. However, over-testing is common and can lead to result misinterpretation, unnecessary heparin avoidance, and increased cost. When there is concern for HIT, guidelines from the American Society of Hematology recommend calculation of the 4Ts score to determine the need for laboratory testing. The Choosing Wisely® initiative recommends against laboratory testing in patients with a low probability score of ≤3. In patients with an intermediate or high probability score (≥4), screening with enzyme-linked immunosorbent assay (ELISA) is performed first. If positive, the diagnosis of HIT is confirmed with a functional assay, commonly the serotonin release assay (SRA).
Methods: In an effort to increase recognition of HIT, providers at a large academic medical center received a non-interruptive alert in the electronic medical record (EMR) on all patients in whom the platelet count declined by ≥50% starting in Aug 2017. We performed a retrospective evaluation of 1) the number of alerts and 2) all ELISA results obtained with or without an alert, over a 90-day period (Dec 2019 to March 2020). A 4Ts score was calculated by chart review by the first author in real-time as the alert was sent (blinded to ELISA and SRA results). Among those patients with multiple alerts or test orders, the first instance was used for analysis. Demographic and clinical characteristics were reported using frequencies and percentages, means (standard deviation, SD), and medians (interquartile range, IQR). Patients with alerts and ELISA testing ordered were compared with 2 groups: 1) patients with alerts but no ELISA ordered; 2) patients with no alerts but ELISA ordered. Comparisons were performed using chi squared tests, Fisher's exact tests, t-tests and Wilcoxon rank-sum tests as appropriate.
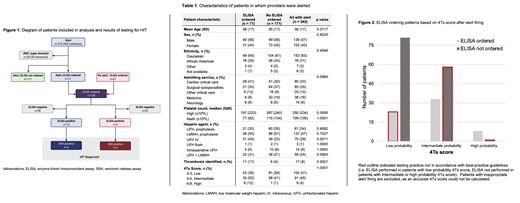
Results: In the 90-day observation period, 302 alerts were fired in 270 patients (Figure 1). Thirty alerts (28 patients, 10%) were generated for patients admitted for organ donation or post-stem cell transplantation, for whom platelet count decline was expected. Excluding these patients, there were 272 alerts in 242 patients (approximately 3 alerts per day in a 1,157-bed hospital). Of patients with alerts, 22 (8%) had a platelet count inaccuracy (i.e. platelets clump or another reason) and 18 (7%) did not receive heparin prior to platelet decline, for a cumulative total of 40 (15%) inappropriate alerts.
In patients with an alert, the ELISA was ordered more frequently for those with a lower platelet nadir (77x10 9/L vs. 115x10 9/L, p<0.0001) or in those with a thrombotic event (11 patients (17%) vs. 6 patients (4%), p=0.0021) (Table 1). Those without an ELISA ordered were more likely to have a low 4Ts score (23 patients (36%) vs. 81 patients (58%), p<0.0001).
In addition to 71 patients with an alert, an ELISA was also ordered for 67 patients without an alert (n=138) (Figure 1). Close to half of ELISA-tested patients had a low 4Ts score (n=51, 46%) (Figure 2). In patients with an alert and ELISA not ordered, 18 (27%) had an intermediate or high 4Ts score.
Seven patients were diagnosed with HIT based on a positive SRA, 6 with an alert and 1 without. The alert demonstrated a sensitivity of 86% (95% CI, 59.8-100%) and specificity of 50% (95% CI, 41.8-58.9%) with a positive predictive value of 0.0845 (95% CI, 0.0198-0.1492) and negative predictive value of 0.9851 (95% CI, 0.9560-1.0000).
Conclusion: An EMR alert based on platelet count decline had multiple shortcomings including frequent inappropriate firings and a lack of guidance on appropriate indications for testing. This evaluation of institutional testing practices indicates frequent use and misinterpretation of ELISA discordant with evidence-based guidelines. Although prompt diagnosis of HIT is important, alternative strategies for identification of at-risk patients and communication of recommended actions to providers should be considered. Because the 4Ts score includes variables difficult to automate in the EMR, our institution is exploring electronic consultation and real-time expert provider access to overcome these limitations.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal